
What Is Outcome Measurement? A Clinician's Practical Guide
Team Meloq
Author

Imagine trying to repair a complex engine with no diagnostic tools. Or attempting to guide a ship across an ocean without a compass. You might make some progress based on intuition, but you’re essentially operating blind. That’s what clinical practice can feel like without proper outcome measurement.
In physiotherapy and sports rehabilitation, outcome measurement is the systematic process of tracking a patient's progress to determine the effectiveness of an intervention. It moves us away from guesswork and provides tangible, objective data to inform and validate our clinical decisions.
Creating a Roadmap for Recovery

Think of it as creating a personalized roadmap for each client, guiding them from their initial injury back to full function or peak performance. It’s a structured approach that uses specific, standardized tools—from validated questionnaires to advanced digital devices—to capture snapshots of a person's condition at different points in time (1).
This process isn't about ticking boxes for administrative purposes. It’s about asking and answering the fundamental questions that lie at the heart of effective, evidence-based care.
By systematically measuring outcomes, clinicians can move beyond subjective impressions and base their treatment adjustments on objective evidence. This is crucial for demonstrating the value of physiotherapy interventions to patients, insurers, and other healthcare stakeholders (2).
Why a Systematic Approach is Non-Negotiable
The purpose of outcome measurement is to provide a structured, repeatable way to evaluate change. Without it, clinicians are left relying on their own perceptions or a patient's vague feeling of being "a bit better." While that feedback is important, it lacks the precision needed for high-quality care.
Outcome measurement introduces objectivity. It relies on tools that have been rigorously tested and validated, ensuring the data we collect is both consistent and meaningful. For example, knowing a patient’s knee flexion improved by exactly 15 degrees is far more powerful and actionable than just noting it has "improved a lot."
The Key Questions It Answers
At its core, this practice helps us answer several critical questions for any rehabilitation or training program:
- Where are we starting from? It establishes a clear, undeniable baseline right at the beginning of care.
- Is what we're doing actually working? Regular measurements clearly show if the client is progressing, hitting a plateau, or even regressing.
- How do we know when we're done? It provides data-driven goalposts for a safe discharge or a confident return to sport.
Let's break this down further. The table below outlines how these core questions translate into day-to-day practice in physiotherapy and sports rehabilitation.
The Core Components of Outcome Measurement at a Glance
| Core Question | What It Means for Clinicians | Example in Practice |
|---|---|---|
| Where is the starting point? | Establishing a baseline to quantify the initial problem and set realistic goals. | Using a goniometer to record a client's shoulder flexion at 95 degrees post-surgery. |
| Is the intervention effective? | Tracking changes over time to justify continuing, modifying, or stopping a treatment. | Re-testing hamstring strength every 2 weeks to see if a new exercise protocol is working. |
| Have the goals been met? | Using objective criteria to determine when it’s safe to discharge or advance to the next phase. | Confirming a client has achieved 90% limb symmetry index on a hop test before clearing them for sport. |
As you can see, each stage of the journey is guided by real data, not just intuition.
By integrating the right tools, we can track everything from a client's pain levels and functional capacity to their raw strength and dynamic balance. Strength is one of the most fundamental metrics we measure, and truly understanding its principles is key. To get a better handle on this, you can learn more about force measurement and see how it forms the foundation for so many performance-based outcomes.
Ultimately, mastering outcome measurement helps you refine your clinical reasoning, keep clients engaged with their own progress, and prove the value of your work with credible data.
References
- Swinkels A, van Peppen RPS, Wittink H, et al. Current use and barriers and facilitators for implementation of standardised measures in physical therapy in the Netherlands. BMC Musculoskelet Disord. 2011;12:106.
- Jette DU, Halbert J, Iverson C, et al. Use of standardized outcome measures in physical therapist practice: perceptions and applications. Phys Ther. 2009;89(2):125-135.
Why Measuring What Matters Became a Game Changer
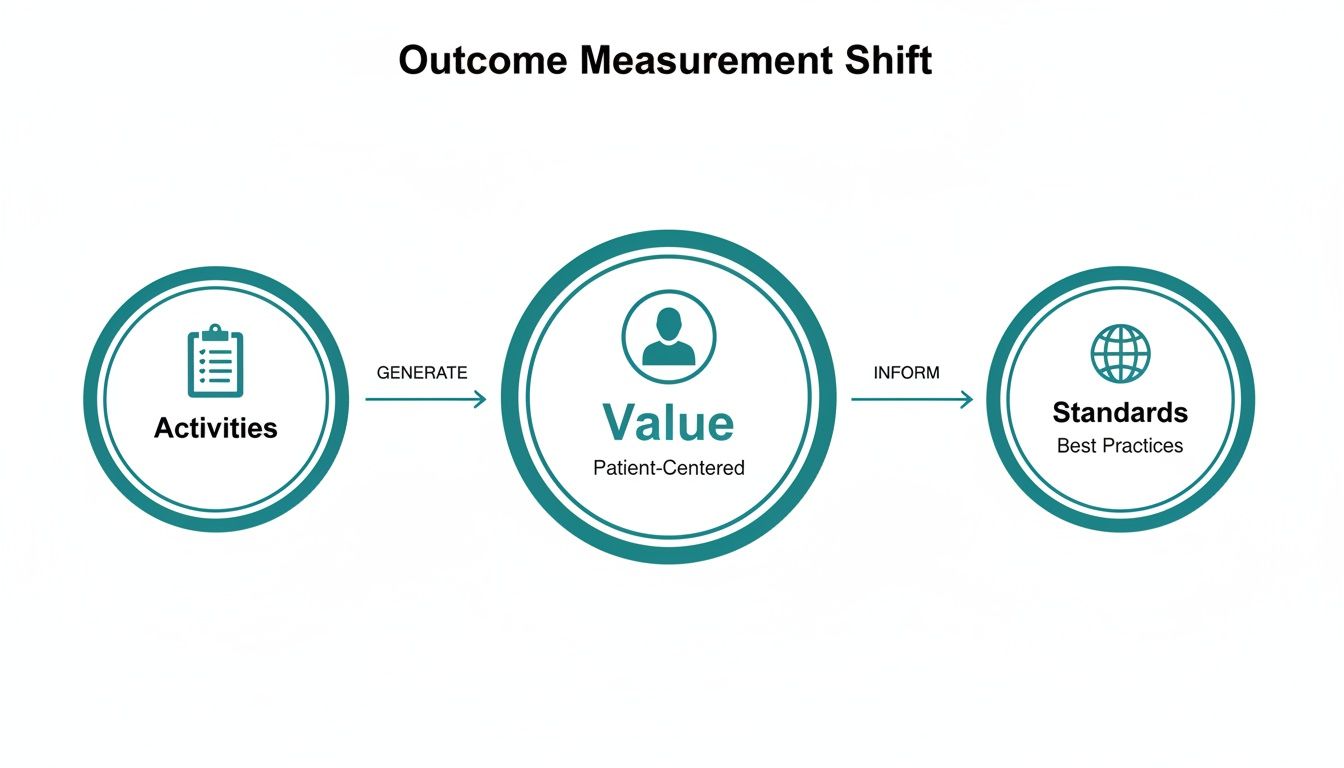
To really appreciate why outcome measurement is so significant, one has to look back at a major shift in how we think about healthcare. We moved from simply counting activities to measuring actual results. For decades, the focus was often on volume—how many physiotherapy sessions a patient completed or how many procedures a clinic performed. While easy to track, that approach tells you next to nothing about whether the patient actually improved.
This shift happened because we recognized a significant flaw in the old model. A patient could attend twenty sessions, but their pain and function might not improve at all. If you're not measuring the outcome, the true value of the care you're providing remains unknown. That realization sparked a much-needed move toward accountability and patient-centered results.
The Rise of Value-Based Healthcare
One of the biggest drivers of this change was the concept of value-based healthcare. This framework redefined what success looks like. It's not about the quantity of services delivered, but the health outcomes achieved relative to the cost. It forced everyone to ask a simple but powerful question: "Are we making a real, meaningful difference in our patients' lives?"
This new focus required a much more systematic way of capturing patient progress. It was no longer enough to say you provided an intervention; you had to demonstrate it worked. This is the point where outcome measurement went from being an academic idea to a clinical necessity.
Outcome measurement became the backbone of evidence-based practice. It provided the objective data needed to compare different treatments, sharpen clinical guidelines, and ensure we’re investing in therapies that deliver real, measurable benefits for patients.
Standardizing a Global Language for Health
As this movement gained momentum, a new challenge appeared. If every clinic, hospital, or country measured success differently, how could we possibly compare results? This led to a global push for standardization, with influential organizations working to create a common language for health outcomes.
This push to standardize was a significant undertaking in the late 20th and early 21st centuries, as healthcare systems aimed to move from activity-based reports to results-based accountability. The International Consortium for Health Outcomes Measurement (ICHOM) played a key role, aiming to publish standardized sets of outcomes for various conditions. Their goal was to enable meaningful comparisons and identify best practices globally. You can explore the history of outcomes measurement to see just how far we've come.
This mission was never just about collecting data; it was about building a foundation for better care everywhere. By agreeing on what to measure and how to measure it, the global healthcare community could finally start comparing apples to apples. This allows us to spot best practices, drive innovation, and ultimately, raise the quality of care for everyone. Outcome measurement isn't just a clinical trend—it's a foundational movement built on evidence, accountability, and a relentless focus on the patient.
The Different Tools in Your Measurement Toolkit
When it comes to tracking progress in rehabilitation and performance, there’s no single "magic bullet" tool. Think of it more like having a well-stocked toolkit, where each tool has a very specific job. By combining different types of outcome measures, you get a complete, 360-degree view of your client's condition—from how they feel to what they can actually do.
This approach reflects a fundamental shift in healthcare. We've moved away from simply tracking activities and are now focused on patient-centered value and global standards of care.
This evolution is why having a varied toolkit is so crucial. It’s what allows us to capture that patient-centered value that defines modern, effective practice. Let’s unpack the main categories of tools you'll be using.
Capturing the Patient's Voice with PROMs
The most important perspective in any recovery journey is always the patient’s. Patient-Reported Outcome Measures (PROMs) are designed to capture exactly that. These are typically validated questionnaires or surveys where patients report on their pain, daily function, symptoms, and overall quality of life.
PROMs are invaluable because they quantify a subjective experience. A client might appear to be moving better, but a PROM can reveal that their pain during daily activities is still a significant barrier.
Common examples include:
- Numeric Pain Rating Scale (NPRS): The classic "rate your pain from 0 to 10" scale.
- Lower Extremity Functional Scale (LEFS): A survey asking patients to rate their difficulty with activities like walking, squatting, or running.
- Disabilities of the Arm, Shoulder and Hand (DASH): A questionnaire focused on upper-limb function and symptoms.
The Clinician's Expert Assessment: CROMs
Next in the toolkit are Clinician-Reported Outcome Measures (CROMs). These are the assessments where you, the therapist, use your clinical skills and often simple tools to measure a specific impairment. This is where your hands-on expertise really shines.
Unlike PROMs, CROMs provide objective data based on your direct evaluation. A perfect example is using a goniometer to measure joint range of motion. You get a precise number that isn’t colored by the patient’s perception.
Seeing Function in Action with Performance-Based Measures
While PROMs capture perception and CROMs measure specific impairments, Performance-Based Measures test a patient's ability to perform a specific physical task. These tests are the bridge between an isolated joint measurement and real-world function.
Here, the patient has to actually do something, which you then time, count, or measure. They are fantastic for setting functional goals and are critical for making decisions on readiness to return to sport or daily life.
Performance-based tests provide a clear, objective snapshot of a client’s functional capacity. A successful 30-Second Sit-to-Stand test, for instance, offers powerful evidence of improved lower body strength and endurance.
Objective Data with Instrumented Measures
Last but not least, Instrumented Measures involve using technology to capture highly precise, objective data that the human eye simply can't. These tools take subjectivity out of the equation and give you hard numbers for strength, balance, and power.
Handheld dynamometers, for instance, provide an exact reading of muscle force in newtons or pounds, which is far more reliable than manual muscle testing grades. Likewise, force plates can measure subtle asymmetries in balance or jump height with incredible precision. This level of detail is essential for high-level athletes and complex rehabilitation cases where small deficits can make a huge difference.
Comparing Different Types of Outcome Measures
To bring it all together, each of these outcome measures provides a different piece of the puzzle. Using them in combination gives you the most complete picture of your client's status and progress.
| Measure Type | What It Measures | Example | Best For |
|---|---|---|---|
| Patient-Reported (PROM) | The patient's subjective experience of pain, function, and quality of life. | Numeric Pain Rating Scale (NPRS) or the LEFS questionnaire. | Understanding the patient's personal experience and how their condition impacts their daily life. |
| Clinician-Reported (CROM) | Objective impairments measured directly by the clinician. | Goniometric measurement of knee flexion range of motion. | Quantifying specific physical limitations like range of motion, strength, or swelling. |
| Performance-Based | A person's ability to perform a specific functional task. | 30-Second Sit-to-Stand Test or the Y-Balance Test. | Assessing real-world function, setting functional goals, and making return-to-sport decisions. |
| Instrumented | Highly precise, objective data on force, balance, or movement. | Handheld dynamometry for strength or force plate analysis for jump height. | High-level performance testing, identifying subtle asymmetries, and research-grade data collection. |
Ultimately, a multi-faceted approach isn't just best practice—it's essential for delivering care that is both evidence-based and genuinely centered on the individual in front of you.
How to Choose Measures You Can Trust
Just because a tool provides a number doesn't automatically make it useful. In the world of outcome measurement, the quality of your data is everything.
Choosing a measure that isn't fit for purpose is like trying to navigate with a faulty compass—the readings might look convincing, but they could lead you in the wrong direction.
To ensure the data you collect is accurate, meaningful, and genuinely useful for guiding treatment, every outcome measure must pass a few critical tests. These are known as its psychometric properties, which is a technical way of asking how trustworthy a measure is. The three main properties you need to understand are validity, reliability, and responsiveness.
Validity: Does It Measure What It Claims To?
Validity is the absolute bedrock of any good outcome measure. It answers one simple, fundamental question: "Is this tool actually measuring what it's supposed to measure?" If a test lacks validity, any data it produces is questionable (1).
Imagine you’re using a new dynamometer to test a client’s quadriceps strength, but it's accidentally picking up force from their hip flexors. That tool would not be a valid measure of isolated quad strength because it's measuring the wrong thing.
A valid tool has been scientifically proven to accurately assess a specific construct. For example, researchers have shown that scores on the Lower Extremity Functional Scale (LEFS) genuinely reflect a person's real-world functional ability, making it a valid tool for that purpose. Ensuring validity is the first critical step to building a clinical picture you can trust.
Reliability: Can It Produce Consistent Results?
Next up is reliability. This one is all about consistency. If you measure the same thing multiple times under the exact same conditions, do you get a similar result? A reliable tool produces consistent, repeatable data, time after time.
Consider measuring grip strength with a dynamometer.
- A reliable device will show you a similar force reading if you test the same person twice in a row, under the same conditions.
- An unreliable device might show a large, random variation between tests, making the data useless for tracking any real change.
In a clinical setting, this is non-negotiable. Reliability ensures that any change you see in the numbers is from a real change in the patient, not just a random error in your measurement. This applies whether it's two different therapists getting the same range of motion reading (inter-rater reliability) or you getting the same reading twice in a row (intra-rater reliability).
Responsiveness: Can It Detect Meaningful Change?
Finally, we have responsiveness, which is also known as sensitivity to change. This property tells you whether a tool can actually detect small but clinically important changes in a patient's condition over time (2). A measure might be valid and reliable, but if it isn't responsive, it's not very helpful for tracking progress.
For instance, a simple "yes/no" questionnaire about knee pain isn't very responsive. A patient’s pain could decrease significantly, but they might still have to answer "yes."
A more responsive tool, like a 0-10 Numeric Pain Rating Scale, can capture that subtle improvement when a patient’s score drops from an 8/10 to a 6/10. This ability to detect real, meaningful change is what makes an outcome measure truly powerful in a rehabilitation setting.
These three properties—validity, reliability, and responsiveness—are the pillars of trustworthy measurement. When you're picking your tools, always look for evidence from peer-reviewed research that they check these boxes. This is especially crucial when using data to make important decisions, like comparing a client’s performance to established benchmarks.
For a deeper dive into that process, it's worth learning about what is normative data and how it adds powerful context to your measurements. At the end of the day, choosing a validated, reliable, and responsive tool ensures your clinical decisions are built on a foundation of solid evidence.
References
- Portney LG, Watkins MP. Foundations of Clinical Research Applications to Practice. 3rd ed. Pearson/Prentice Hall; 2009.
- Terwee CB, Bot SDM, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34-42.
Putting Standardized Measurement into Practice
We all agree on the big picture: creating a common language to evaluate patient progress and treatment effectiveness. It’s an ambitious, powerful goal. But when you try to bring that ideal down to the ground level of a busy clinic, you can quickly discover a significant gap.
Knowing what outcome measurement is and actually doing it consistently are two very different things. For those of us in physiotherapy, sports rehabilitation, and performance conditioning, the day-to-day realities of implementation can feel overwhelming. The ambition is there, but it often collides with a packed schedule and the unique needs of every individual walking through the door. This disconnect is a well-known hurdle in our field.
The Real-World Barriers to Adoption
It's not for a lack of trying. Clinicians and organizations want to adopt standardized measures, but they run into practical roadblocks that are all too familiar to anyone on the front lines of patient care. Acknowledging these hurdles isn't about making excuses—it's the first step to finding a way around them.
A few key barriers pop up time and time again, both in the clinic and in scientific literature:
- Time Constraints: This is a major factor. Properly administering multiple outcome measures, logging the data, and then interpreting it takes time—a resource that’s always in short supply during a patient appointment.
- Cost and Resources: Bringing in new tools, like digital dynamometers or force plates, requires a budget. There is also the cost of training staff to use the equipment correctly and consistently.
- Lack of Consensus: With thousands of outcome measures available, just picking the "right" one can feel paralyzing. Different professional groups or even clinicians in the same practice might have conflicting preferences, which makes getting everyone on the same page a challenge.
The real challenge isn't just about collecting data. It's about weaving a new process into an already complex workflow. Success hinges on getting buy-in from the entire team—from the front desk to the senior therapists—and having a clear plan for how this data will actually be used to guide patient care.
The Standardization Gap in Scientific Literature
This isn't just a clinical hunch; it's a well-documented problem. Despite the clear benefits of a unified approach, large-scale studies have confirmed that consistent implementation remains a significant challenge. The absence of a universal standard creates difficulties for research and makes it tough to compare one clinic's results to another.
For example, systematic reviews over the last decade have consistently found that the use of standardized outcome sets in clinical settings is variable. There's often so much variation in what gets measured from one clinic or study to another that comparing results or pooling them for larger analyses becomes nearly impossible. This inconsistency is a major roadblock. As researchers often point out, it undermines our ability to compare different treatments across countries and over time.
Moving Forward with Practical Solutions
Pointing out these barriers isn't admitting defeat. It's about being realistic so we can find practical solutions that work in a modern clinic. Getting past these hurdles means taking a strategic approach that balances the ideal of perfect data with the reality of daily practice.
The key is to start small and be smart about it. Focus on implementing just one or two highly relevant, validated, and efficient measures first. Build momentum by showing your team—and your patients—how this data leads directly to better, more personalized treatment plans. The road to standardization isn't a sprint. It’s a deliberate process of integrating meaningful measurement into the heart of what you do every day.
The Future Is Objective, Repeatable Data
Looking ahead, the conversation around outcome measurement is no longer about if we should collect data. It’s about how we can do it better, faster, and more accurately. Technology is leading the charge, making it easier than ever to gather the kind of objective, repeatable data that was once mainly confined to university research labs. This shift is finally closing the gap between what we want to achieve in the clinic and what's actually possible day-to-day.

Digital tools, from instrumented dynamometers to wearable motion sensors, are becoming the new standard of care. They excel at standardizing testing protocols—which is essential for making sure a measurement taken today is directly comparable to one taken next month. By reducing subjective error and clinician variability, these devices deliver a level of consistency that manual methods often cannot match.
Empowering Clinicians and Patients with Data
One of the great advantages of this tech-driven approach is the immediate feedback. When a patient sees their strength output jump by 10% on a digital display or tracks their improving range of motion in an app, the vague idea of "getting better" becomes a concrete reality. That instant, visual proof is a powerful motivator that keeps people engaged and invested in their own recovery.
It changes the dynamic in the clinic. Instead of relying only on the clinician's interpretation, both parties can look at the objective numbers together. This builds a more collaborative and transparent relationship. You can read more about how technology is reshaping our field and check out the future of physical therapy.
This move towards objective data isn’t just about better individual care; it’s about contributing to a larger pool of high-quality information. Standardized data allows us to see what works, for whom, and under what conditions, pushing the entire field forward.
From Individual Progress to Global Health Insights
The real power of standardized, objective data becomes apparent when you zoom out. When thousands of clinicians collect comparable data, we can start answering the big questions about treatment effectiveness, injury trends, and population health. It transforms individual clinical encounters into valuable data points that can inform global health initiatives.
By embracing objective and repeatable data collection, we don't just fine-tune our individual treatment plans. We contribute to building a smarter, more evidence-based healthcare system for everyone.
Putting It All Into Practice: Your Questions Answered
Diving into outcome measurement can bring up a few practical questions. Let's tackle some of the most common ones that come up in the clinic to clear the path for your implementation.
How Often Should I Measure Outcomes?
The optimal frequency depends on the patient's condition, the clinical setting, and the measure itself. However, a solid rule of thumb is to measure at the initial evaluation to establish a baseline, check in at regular intervals (e.g., every 2-4 weeks), and then measure again at discharge to quantify progress (1).
For someone with an acute injury, you might need to measure more often to ensure the treatment plan is on track. In a performance setting, you would likely measure before and after a specific training block to evaluate its effectiveness. The key is consistency—whatever schedule you pick, stick with it.
Can I Use the Same Outcome Measures for Every Patient?
It's tempting to find a few tools you like and use them for everyone, but this can lead to less meaningful data. The best approach is always to choose measures that are valid and reliable for the specific condition and population you're working with.
For example:
- For a patient with a rotator cuff repair, the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire is a suitable tool.
- For someone rehabilitating an ACL reconstruction, the Lower Extremity Functional Scale (LEFS) is a much better fit.
Picking the right measure for the right person ensures you're asking the right questions and tracking what truly matters for their recovery.
What if a Patient's Subjective Report Contradicts Objective Data?
This happens all the time, and it’s not a problem—it's a clinical opportunity. A patient might say they feel much better (a great PROM score), but their objective strength numbers haven't changed. This isn't a contradiction; it's a crucial insight into their recovery.
This scenario illustrates the multi-faceted nature of recovery. It likely means your interventions have successfully reduced their pain or boosted their confidence—a significant win. At the same time, it clearly signals that an underlying strength deficit may still exist and needs to be our next focus before they can safely return to full activity.
Instead of seeing a conflict, see an opportunity to educate your patient. You can validate their experience—"It's great that you're feeling so much better!"—while explaining why building that foundational strength is the next critical step for a durable recovery. It shows them you're looking at the whole picture, which is what great outcome measurement is all about.
Ready to swap subjective guesswork for objective, repeatable data? The Meloq ecosystem of digital measurement tools—including the EasyAngle goniometer and EasyForce dynamometer—is built for busy clinicians who demand both accuracy and efficiency. Standardize your assessments, engage your patients, and prove your value with data you can stand behind. Explore the Meloq device ecosystem.